Recently declared a nationwide public health emergency, the misuse and abuse of opioids in the United States takes the lives of more than 90 Americans every day.¹ The most recent report from the US Centers for Disease Control and Prevention (CDC) recounted more than 65,000 deaths from drug overdose over a 12-month period—a record high.² More alarming, however, is that drug overdose deaths have increased every year since 1999, mirroring a similar trend in increased opioid sales.³˒ ⁴ In fact, both the amount of prescription opioids sold and overdose deaths involving opioids have more than quadrupled since 1999.⁴ As one of the most commonly prescribed medications to the 100 million patients experiencing chronic pain in the United States annually, opioids are integral to many pain management practices.⁵ ˒⁶ With the national spotlight increasingly focused on the hazards of opioid misuse, however, the time is now to find additional solutions that may assist in pain management.
While a plethora of addiction screening, education, and prevention programs have been instituted in pain management practices,⁷˒ ⁸ nonpharmacalogical treatment modalities have the potential to make chronic pain care safer. In response to the opioid crisis, one such program mandates that patients who need opioids for nonmalignant pain must first see a psychotherapist to assess suicide risk, and provide psychological support and stress reduction. In addition, these patients must also see an addictionologist to assess risk for addiction. Finally, this opioid safety model includes “non-drug” approaches to pain management, including exercise, physical therapy, and integrative medicine treatments.⁹ Overall, there are a wide range of chronic pain treatment strategies, including pulsed electromagnetic field (PEMF) therapy.
Clinical Efficacy of PEMF
Recent research identifies improvements in the treatment of chronic pain using PEMF therapy. Sutbeyaz et al.¹⁰ tested low-frequency PEMF therapy on 56 women with fibromyalgia. Random group assignment placed 28 women in a PEMF treatment group, while the 28-patient placebo group received a sham therapy. After receiving two 30-minute treatments per day for 3 weeks, researchers reported 52% reduction in life interference in the PEMF group, compared to 11% reduction in the sham group. Overall, participants in the PEMF group reported statistically significant reductions in pain.¹⁰
In an exploratory study of PEMF therapy’s effects on postoperative pain, Hedèn¹¹also reports a three-fold decrease in subjective pain by the PEMF group compared to a placebo after only three days. Another study from 2014 evaluated the effects of PEMF and exercise on pain, muscle functioning, and muscle strength in patients with shoulder impingement syndrome (SIS).¹¹ These 56 patients, randomly assigned to a PEMF plus exercise condition or placebo plus exercise condition, completed a three-week trial. Results indicated significantly higher levels of functioning and reduced pain in the PEMF group. The PEMF group also exhibited greater strength.¹¹
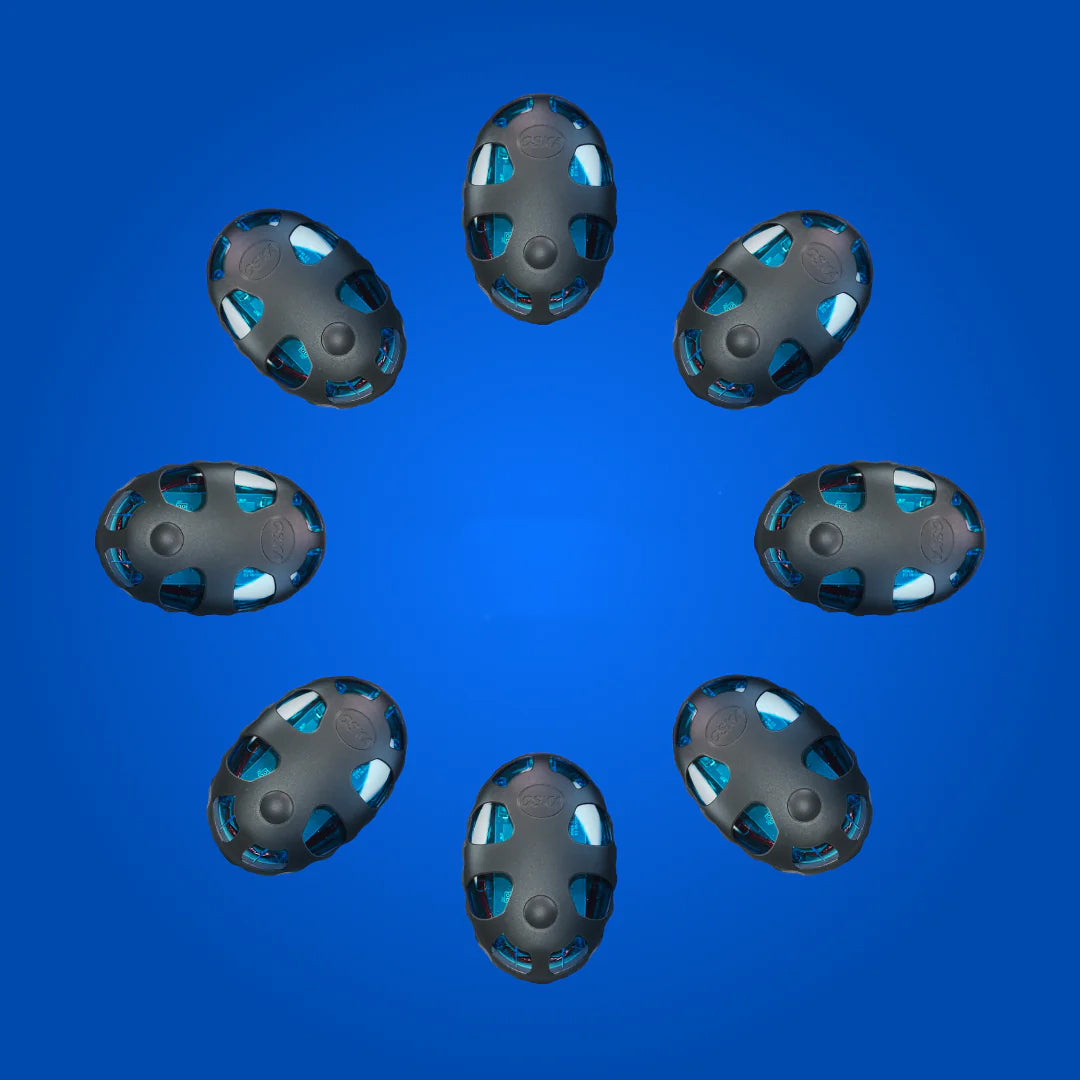
The present study evaluates the effectiveness of PEMF therapy on chronic pain patients as part of a two-week double blind clinical trial with placebo using the OSKA Pulse PEMF device (OSKA Wellness, Carlsbad, CA).¹²
Methods
Participants. Thirty-nine patients (n = 39) with diagnosed chronic knee, shoulder, or back pain were enrolled in the study. To be included, participants were required to be older than 18 years of age, be capable of providing full informed consent, and had to have either chronic should, back, or knee pain. Participants were excluded from the study if they had vestibular disease, epilepsy, cancer, or a pacemaker. Nine patients withdrew throughout the trial for reasons including: lack of pain reduction, inability to follow the protocol, and difficulty using the device. Overall, 30 patients completed the trial.
Design. The trial used a between-subjects design to compare baseline to follow up change in pain between the two groups.
Materials. Each participant was provided a daily log to report their pain, stress, and daily use of the device. Pain and stress scores in daily log were based on a 10-point Likert scale (0 = no pain/stress, 10 = extreme pain/stress). Participants were sent home with either an OSKA Pulse or a sham device. The sham device looked and functioned the same as the actual device, but did not emit any PEMF waves.
Procedure.Both patients and investigators were blinded as to real or placebo OSKA device. Each participant was randomly assigned to either the OSKA Pulse group (n = 15) or placebo group (n = 15). At intake, after signing full informed consent, each participant was briefed on the protocol. For two weeks, participants used the PEM device or placebo while recording their pain, stress, and number of times using the device in a daily log. For the first seven days, all participants were instructed to use the device four to six times per day for 30 minutes at a time, recording their daily log scores around the same time (ie, after dinner, before bed). For the second week, participants were asked to use the device only two to four times per day for 30 minutes at a time, and record their pain, stress, and usage in the daily log.
Upon completion of the trial, participants returned their devices and daily logs to the clinical trial coordinator. The coordinator manually entered all data points into excel, using a data analysis package to run between-subjects one-tailed t-tests. Assuming no detrimental side effects of the PEMF device Pulse, the authors chose a one-tailed t-test to evaluate pain and stress scores. This one-directional test focuses on improvements in pain conditions.
Results
A one-tailed between subjects t-test was performed to evaluate mean group differences in changes in pain and stress after days 7 and 14. After 7 days, the OSKA Pulse group reported a slight decrease in pain (MOska Pulse = -0.455, SDOska Pulse = 1.57), while the placebo group reported a small increase(MPlacebo = 0.091, SDPlacebo = 1.44). Group differences were nonsignificant; t(20) = .847, p = .20). Further analysesshowed significantly greater pain reduction in the Oska Pulse group (MOska Pulse = -0.9, SDOska Pulse = 1.14)compared to the placebo group (MPlacebo = -0.09, SDPlacebo = 0.7) after 14 days; t(17) = 2.03, p = .029. See Figure 1. Group comparisons of stress produced no differences after day 7 or day 14.
Conclusion
This double-blind clinical trial with placebo provided information on the efficacy of PEMF therapy in treating chronic pain. There was significantly more reduction in pain in the OSKA Pulse group after 14 days of use than placebo. These results suggested that the OSKA Pulse may be an effective tool in pain attenuation. Data analyses showed interesting trends in subjective pain scores, including a slight increase in pain in the placebo group after day 7, while the OSKA Pulse group, on average, reported a decline in pain intensity.
This trial encountered some limitations. Incomplete trials and participant attrition, though expected, eliminated a number of participant datasets from analyses. These exclusions from analyses decreased statistical power and contributed to lower external validity of the PEMF intervention. Future trials for this device should include larger sample sizes to account for participant dropout. Participants also cited using the OSKA Pulse 4-6 times per day as a possible drawback.
Results suggest the need for further research on the efficacy of PEMF in pain management, and its possible impact on reducing opioid/pharmacological usage in patients with chronic or complex pain. Such adjunctive pain management solutions may be useful in the treatment of certain pain conditions.
Editor's note: In January 2019 Oska Pulse released the Enhanced Oska Pulse, which features 90-minute run sessions and 20-hour battery life allowing users more flexibility and convenience when wearing the device
Source: https://www.medcentral.com/pain/treating-chronic-pain-using-oska-pulse-device